On a late September night in the American Midwest, the glass tower of Ridgeview Medical Center glowed against the sky like a lighthouse no one trusted anymore, a place where the bright red EMERGENCY sign promised help while something far darker ruled the corridors inside.
James Comolmes had slapped nurses before. Dozens of times, if anyone had been brave enough to keep count. His hand always moved fast, the way it had that first week after he took over as Chief Executive Officer of Ridgeview Medical, a nonprofit hospital system just outside Columbus, Ohio. On paper, Ridgeview was a model of modern U.S. healthcare: trauma center, cardiac program, helicopter pads, affiliations with a major state university. In glossy brochures, patients smiled under soft lighting and words like excellence and compassion floated beside the photos.
Inside, the people who worked there knew better.
In boardroom portraits and press releases, James looked like the kind of leader hospital boards loved to hire. Dark, precisely cut hair, a tailored suit that always fit just right, a tie that never seemed to wrinkle, and a smile that sat comfortably beneath his polished features. He spoke fluently about quality metrics, payer mixes, reimbursement cuts, Medicare and Medicaid pressure, and “the challenges of American healthcare.” He knew the language of Washington, D.C. policy briefings and understood which phrases sounded good on local news.
To the nurses in the halls of Ridgeview, he was something else entirely.
The first time he slapped someone at Ridgeview, he did it in a hallway just outside Conference Room B on the administrative floor. A young nurse named Jennifer had been told to bring updated lab results to the philanthropy meeting. She didn’t realize the meeting was still in progress when she pushed the door open and stepped inside with a folder clutched in her hand.
James looked up from the table where he sat flanked by donors in suits and elegant dresses. His eyes narrowed, then softened into a charming smile for the guests.
“Excuse me a moment,” he said.
He walked into the hallway with Jennifer, closing the door behind them with a quiet click. She began to apologize, stumbling over words about miscommunication and timing. The apology never finished. His hand came up in a single smooth motion and landed with a sharp, flat sound against her cheek. It wasn’t strong enough to send her sprawling. It didn’t leave visible marks that would photograph clearly. But the way her head snapped to the side, the stunned breath that broke in her chest, the tears that sprang into her eyes—that was enough.
“Learn the difference between an open door and an invitation,” he said calmly, as if correcting a charting error. “Ridgeview is not a playground. You want to keep your job? Use your head.”
Then he opened the conference room door, put his polished smile back on, and resumed his presentation about strategic growth in the U.S. Midwest healthcare market.
Jennifer did what many people in American workplaces do when a line is crossed so blatantly she could hardly believe it had happened. She wrote it up. She went to Human Resources. She used words like inappropriate contact, physical aggression, intimidation. She believed, for about forty-eight hours, that the system would protect her.
Ridgeview’s HR department opened what they called a “formal review.” They took her statement. They nodded with sympathetic eyes and professional empathy. They interviewed a few people. They spoke with James behind closed doors.
James’ version was that Jennifer had been unstable, overheated, irrational after he corrected her tone. He insisted he had simply raised his hand in a calming gesture and she had overreacted. The donors, when called later, politely claimed they hadn’t seen anything in the hallway. They remembered a brief conversation, nothing more. Perhaps the young nurse had misinterpreted a stern gesture as something else in a moment of stress. These things happen.
Jennifer was eventually called back to HR. She was told the evidence was inconclusive. She was reminded of how much Ridgeview had invested in her orientation. Then she was offered a modest settlement and a non-disclosure agreement detailing the terms. She could leave quietly with a check and a neutral employment reference, or she could stay and continue working under a CEO who now knew she had tried to report him.
Jennifer signed. She left nursing. The document with her signature went into a secure file that never appeared in any board presentation or Joint Commission audit. The slap never made it into any safety report or quality dashboard. It existed only in Jennifer’s memory and in the private confidence of a few nurses who whispered about it during night shifts.
After that, the slaps came more easily.
They weren’t daily, or even weekly. They arrived like storms in summer, rolling in from a clear sky, unpredictable but somehow no longer surprising. A charge nurse who spoke up about staffing assignments during a respiratory virus surge. A medical assistant who handed him the wrong printout. A respiratory therapist who politely insisted a patient needed more time on a ventilator before transfer. A quiet, almost invisible pattern spread through the hospital: sudden violence, quick denials, brief “investigations,” settlements, and silence.
The board of directors, meeting four times a year high above the city, saw none of this. They saw financial charts. They saw improved margins in a brutal U.S. healthcare environment. They saw growth in commercially insured admissions. They saw Ridgeview climb in regional rankings. They heard James explain cost controls, productivity targets, lean initiatives, and payer negotiations with confidence and precision.
For the nurses on the floors, the real policy was simpler: stay small, stay quiet, survive.
By the time Clara Jensen’s résumé appeared in the HR inbox, James had been in charge for nearly five years. Twelve nurses had been struck in one way or another. Dozens had been humiliated in front of colleagues. Many more had left, worn out, broken down, or simply unwilling to keep showing up in a place where dignity felt optional.
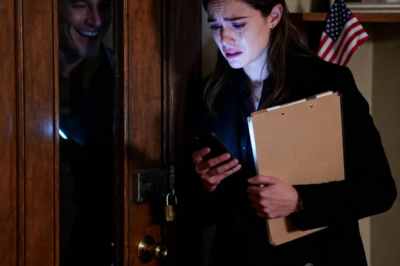
Clara walked into Ridgeview Medical Center on a Monday morning in early September, when the Ohio summer was finally loosening its grip and the air outside carried the first hint of coolness. The American flag at the entrance fluttered in a light breeze over a row of parked cars: minivans, pickup trucks, compact sedans with out-of-state plates. Ambulances idled near the emergency bay, their engines low and steady. On the roof, the hospital’s helipad glowed faintly against a pale sky.
She moved through the hospital’s main lobby with a canvas bag over one shoulder, wearing simple scrubs and comfortable shoes. Her hair was pulled back. Her face was calm, almost soft. To anyone watching, she looked like every other nurse starting a new job in an American hospital: polite, slightly cautious, ready to blend into a system that would demand too much from her and pay too little in return.
The security officer at the entrance checked her ID badge and noticed her name, her birth year, the Ohio address on the form. Nothing remarkable. He joked about how chilly the winters could get in the Midwest and asked if she was ready for it. She answered with a small smile and said she’d seen worse.
He had no idea how true that was.
Upstairs, on the medical–surgical unit, the nurse manager flipped through Clara’s file before orientation. Ten years of nursing experience. Critical care certification. A history of work at a community hospital two states away. Excellent references. A brief but clearly documented mention of prior service in the U.S. Marine Corps before nursing school. That alone made the manager raise an eyebrow; it wasn’t every day a former Marine ended up working bedside in a place like Ridgeview. But the résumé looked solid, and finding experienced nurses who were still willing to work in hospitals had become harder every year in the United States.
During orientation, Clara listened carefully as the unit manager went over policies and protocols. No cell phones at the bedside. Mandatory documentation for pain reassessments. Medication scanning procedures. Chain-of-command steps. She wrote notes in a neat, precise hand, the kind that made charts easy to read and nursing instructors proud.
When the manager mentioned “high expectations from the CEO” and a “very hands-on leadership style,” Clara let her pen pause for a moment, then resumed writing as if the phrase meant nothing more than extra meetings.
The manager didn’t use James’ name. She didn’t talk about slaps or shouting or the day someone saw him slam his hand down on a desk so hard a coffee mug broke. She said only that professionalism was essential, that concerns should be reported “through proper channels,” that the hospital had “a zero-tolerance policy for harassment,” the kind of words required in American HR manuals and orientation videos.
By lunchtime, word had spread on the unit that there was a new nurse starting. Nurses, like soldiers and teachers and diner cooks, have their own ways of taking measure of a newcomer. One by one, they found reasons to talk to Clara in the break room, in the med room, by the supply closet.
Patricia, an eight-year veteran of Ridgeview’s med–surg floor, was the first to pull her aside. She was the kind of American nurse who’d seen everything: night shifts that stretched into day shifts, back-to-back codes, families melting down at three in the morning, administrators timing bathroom breaks. She had lines at the corners of her eyes that came from smiling at patients and not enough sleep.
“Where’d you work before?” Patricia asked, opening a packet of saltines and sliding half the stack toward Clara.
“Community hospital,” Clara said. “Smaller than here. A couple states over.”
“Ever work in a system like this?” Patricia nodded toward the ceiling, toward the administrative floors where the suits sat.
Clara hesitated just enough to make the pause noticeable, then shook her head.
Patricia glanced at the door to make sure it was closed. Her voice dropped.
“You’re going to hear about our CEO,” she said. “If you haven’t already. People don’t say much during orientation. They never do. But you should know what you’re walking into.”
She told Clara about the hallway outside Conference Room B, about Jennifer’s sudden departure and the whisper of legal papers. She didn’t use the word slapped at first. She said “put hands on,” then “hit,” then finally settled on the word everyone else used quietly when they thought the cameras in the ceiling couldn’t hear.
Other stories followed: a nurse in PACU who’d been yelled at until she shook, an ICU charge nurse who’d been transferred to a lower-paying outpatient role after questioning staffing cuts, a night the CEO had been called about an unstable patient and shown up angrier about the hour than the condition.
“Best way to stay here,” Patricia finished, “is to stay invisible. Don’t give him a reason to notice you. Don’t challenge anything. Don’t contradict him. If he walks down the hall, go the other way. You have bills? You got kids? A mortgage? Then you learn to look at the floor.”
Clara nodded, listening with a stillness that made the other woman feel heard. She didn’t ask many questions. She didn’t gasp or react with the outrage some new hires showed before they either adapted or left. She simply said, “Thank you for telling me. I appreciate it. I’ll be careful.”
It sounded, to Patricia, like the answer of someone who didn’t fully grasp the danger, another nurse who believed professionalism would be enough protection in a place where it never had been.
Patricia walked away thinking she should check on the new nurse over the coming weeks, in case Ridgeview broke her the way it had broken others.
She had no idea that Clara understood danger more precisely than anyone else on that floor.
There were tells, if anyone had known what to look for. The way Clara stood with her weight balanced evenly on both feet instead of slumping into her hips after a twelve-hour shift. The way she always kept a clear line of sight to the door, even when she was sitting in the break room. The way she tracked movement in the hall without turning her head fully, her eyes flicking just enough to register the direction and speed of whoever was passing by.
On her second day, a metal tray crashed to the floor behind her when an orderly fumbled a stack of supplies. Most of the nurses in the area flinched or gasped. A few cursed under their breath. Clara turned, yes, but the movement was smooth and controlled, more assessment than alarm. She checked the source of the noise, judged that no one was hurt, then went right back to programming an IV pump. The way she moved made it clear that loud noises, sudden shifts, unexpected sounds were not unfamiliar to her.
Her skills as a nurse emerged quickly. Within forty-eight hours, it was obvious she knew what she was doing. Her assessments were thorough without being slow. She caught subtle changes in patients—the slight shift in breathing, the tiny delay in answering questions—that signaled trouble before it appeared on monitors. She charted like someone who understood that in American hospitals, documentation was both shield and sword, protection and proof.
She was kind. That was what patients noticed first. She spoke to them in a steady, soft voice, explaining what each medication was for, translating the language of labs and imaging and “protocols” into something a retired teacher or a truck driver’s spouse could understand. She listened when they talked about their lives outside the hospital, about grandkids in Little League or a son stationed overseas or a daughter struggling in college. In a system that often treated people as bed numbers and diagnoses, Clara made them feel human.
But beneath that gentleness was a steel no one understood yet.
James noticed her on her fourth day.
He was walking the medical–surgical corridor on his usual rounds, the ones that made staff melt into doorways and find sudden reasons to check on patients who didn’t need anything. He liked to think of these walks as “visibility,” a way to demonstrate his presence in the clinical environment. In reality, everyone knew they were inspection tours. He watched for mistakes, for clutter, for anything that made the hospital look less than perfect in his eyes.
He saw Clara outside Room 417, a chart tablet in her hands. Her badge flashed under the fluorescent lights: Jensen, RN. He knew he hadn’t seen her face before. New, then. New nurses were either a problem waiting to happen or a fresh slate to mold into his version of “professional.”
She glanced up just as he drew close, met his eyes briefly, and nodded.
“Good morning,” she said. Not deferential, not casual, just even.
Most staff avoided his gaze, staring at the floor or the wall just above his shoulder. Some greeted him with forced enthusiasm, layering their voices with extra brightness. Clara’s tone held none of that. It sounded like she was greeting a colleague, nothing more.
James barely registered it. He was preoccupied with a coming finance committee meeting about Medicare reimbursement and length-of-stay metrics, with a draft email he needed to send to the board chair about a potential partnership with a large insurer. He made a mental note that a new nurse on 4 North didn’t avert her eyes quickly enough, then moved on.
Clara, on the other hand, watched him with the awareness of someone studying an opponent. She noted the way people reacted as he passed—a housekeeping worker who literally stepped into an empty room to avoid him, a pharmacist who stiffened when he entered the unit, a resident physician who laughed too loudly at a comment James made about “physician productivity.”
She noticed how he squared his shoulders just before he criticized someone, how his lips thinned slightly before his voice rose, how he tilted his head when he was about to humiliate someone in a public space. She recognized these signs in the same way she’d once learned to read the posture and eyes of people outside wire fences in hot, dusty places half a world away.
In that first week, there were almost encounters between them—moments when he stepped into a med room she was in and she adjusted her position slightly, making sure the counter wasn’t at her back, leaving herself room to move; a staff huddle where he dropped in unexpectedly and Clara slipped behind a taller nurse, watching without being watched. Each time, she evaluated, calculated, and walked away with more information than he could ever guess.
On her seventh day at Ridgeview, she met Walter Harrison.
Walter was eighty-three years old, a veteran who’d served in Southeast Asia before half the nurses on the unit were born. He had the dry humor of a Midwestern grandfather and the slow, measured movements of someone whose joints had absorbed more than their share of miles. He was recovering from pneumonia, his breath still a little raspy, his oxygen tubing arched over his ears.
When Clara stepped into his room late one afternoon to check his vitals, he watched her the way people who have seen too much watch everyone: quietly, with more attention than he let on.
“You’re new,” he said, when she finished adjusting his pillow.
“Yes, sir,” she replied. “Clara. I’ve been here about a week.”
“You were in the service,” he said, not as a question but as a statement.
She paused. Her fingers tightened a fraction around the blood pressure cuff before she smoothed her expression.
“Yes,” she said. “Marine Corps.”
He nodded slowly, his mouth curving into a small, knowing smile.
“Thought so. You walk like someone who’s been told to hit the ground fast and get back up faster.”
She let herself smile back, just a little.
“Did you serve?” she asked.
“Army,” he said. “Long time ago. Different war. Same country on the paperwork.”
They didn’t say much more about it. They didn’t need to. The connection settled between them like a quiet understanding. Walter watched her leave the room later with an expression that mixed respect and concern, as if he recognized a soldier who had walked into a new kind of battlefield.
James had struck twelve nurses in his career. Walter didn’t know that, but he could sense something like weather about to turn. Clara already knew the number, or close enough. She’d done her research before she ever applied.
On her eighth day, Ridgeview’s emergency department began the shift that would end James’ rule.
It was a typical Friday evening in an American city hospital: full waiting room, a police cruiser parked outside, an ambulance arriving every few minutes with somebody’s worst day inside. The ER screens were filled with names that represented car accidents on icy roads, chest pains in middle-aged men with too much stress and too little sleep, teenagers with sports injuries, elderly women who’d gotten dizzy in grocery store aisles.
Clara had been floated down from med–surg to help cover a staffing gap, something that happened more often now that so many nurses had left. She moved through the controlled chaos with the calm of someone who had triaged on far harsher days in far less controlled environments.
An ambulance arrived with an elderly woman named Dorothy Fletcher. She was in her late seventies, neatly dressed, her gray hair pinned back, lips pale with worry. Her left side felt weak. Her speech was slurred. Her paramedic report said possible stroke, onset time about forty minutes earlier.
The ER attending ordered imaging and labs immediately. A CT scan was needed. So were basic tests. But the scanner was already occupied by a trauma case: a man pulled from a car crushed on Interstate 70. The techs were working as fast as they could. The trauma doctors were fighting for another life.
The delay wasn’t negligence. It was reality. In American emergency departments, resources are finite, even when everything looks shiny and modern. Someone always waits. Someone is always next.
Clara was assigned to stay with Mrs. Fletcher. She monitored her neurological status, checking strength in her limbs, watching her pupils, listening to her speech. She spoke clearly and gently, explaining that the scan was coming, that they were watching her closely, that nothing important would be missed.
Dorothy clung to her hand like it was a lifeline.
In an office upstairs, James received a text from one of the hospital’s board members, a man who owned several local businesses and contributed annually to Ridgeview’s foundation. His wife, Dorothy, had been taken to the ER. He had been told she’d arrived more than thirty minutes ago. He had not been given an update since. He was concerned.
James read the message and felt anger rise before he even finished. He pictured a board member at a cocktail party weeks from now, muttering about a lack of responsiveness, about the gap between Ridgeview’s public claims and private realities. He imagined donors reconsidering their commitments. He thought about reputational risk, not about Dorothy’s fear.
He did not call the attending physician to ask for an update. He did not look at the ER dashboard to see that the CT scanner was occupied with a critical trauma. He did what he always did when he felt his control threatened.
He went looking for someone to blame.
He walked into the elevator with his jaw tight, his thoughts already rehearsing the lines he’d use. There would be raised voices, perhaps a few well-chosen words about incompetence, expectations, accountability. The staff would shrink back. Someone would apologize. He would reassert dominance. Balance restored.
The elevator doors opened to the ER corridor, a space of bright lights and constant noise. As he walked in, the unit coordinator recognized his stride, the specific way he took ownership of the space with each step. Her stomach sank.
She rushed to meet him, trying to intercept him before he reached any individual room.
“Mr. Comolmes,” she began, “we’re working on an update for Mrs. Fletcher right now. The CT scanner is occupied with—”
He brushed past her.
“Why haven’t I heard anything?” he demanded. “The board member’s wife has been down here half an hour with no report?”
“Sir, the trauma in CT—”
“I don’t care about excuses,” he said, his voice rising. “This is not a free clinic. This is a major medical center in the United States. We do not keep board members’ families waiting without communication. Where is the nurse assigned to her?”
The ER physician tried to intervene, stepping into James’ path, starting to explain the clinical triage, the decisions made, the balancing of resources. James cut him off with a sharp gesture.
“I’ll speak to the nurse,” he snapped. “If she can’t manage basic communication, she can find employment somewhere else.”
Clara heard his voice before she saw him. It carried down the corridor, sharp and edged, the kind of voice that made other voices drop. Mrs. Fletcher’s hand tightened around Clara’s fingers.
“What’s happening?” Dorothy whispered. Her words slurred slightly, her eyes wide.
“Just some noise in the hall,” Clara said softly. “You’re safe. I’m right here.”
She shifted her stance without thinking, placing herself more squarely between Dorothy and the doorway. It was a small movement, the kind that could have been about privacy or modesty, but it came from a place deeper than habit.
James appeared at the entrance to the room, his face flushed, his shoulders tight.
“Who’s responsible for this patient?” he demanded.
Clara turned toward him. Her heart rate did not spike. She registered his posture, his tone, the distance between them, the position of the bed rails, the corner of the room behind him, the curtain track overhead. A quick scan, as routine to her as checking a patient’s oxygen saturation.
“I am,” she said.
He stepped forward, eyes snapping to her badge.
“Why hasn’t she been scanned?” he asked. “Do you understand who this is?”
“Yes,” Clara said evenly. “She’s a seventy-eight-year-old woman with suspected stroke symptoms. The CT scanner is currently in use for a trauma patient whose condition is unstable. The attending physician has prioritized cases appropriately. I’m monitoring her closely while we wait, and I’ve been keeping her informed.”
The ER seemed to shrink around them. Conversations dimmed. Nurses glanced over their shoulders. The physician who’d tried to intervene swallowed the words he’d been about to say and watched.
James fixed Clara with a look that had made other people fold.
“You do not lecture me on priorities,” he said. “Your job is to carry out orders, not make decisions above your station. When a board member’s spouse is in our ER, I expect immediate attention and constant updates. Do you have any idea what kind of damage this kind of delay can do to this hospital?”
Clara held his gaze.
“Sir,” she said, “the delay is clinically appropriate. The trauma patient in CT could die without rapid imaging and intervention. Mrs. Fletcher is stable, and she needs a quiet, calm environment. Raising your voice in her doorway is not good for her blood pressure or her neurological status. I would like to continue caring for her.”
A silence fell that was different from the usual ER pauses. This one had weight.
Patricia, at the nurse’s station, felt her throat go dry. She caught Clara’s eye and shook her head slightly: don’t do this. Another nurse whispered Clara’s name under her breath, a warning, a plea.
They all knew what happened when someone spoke to James that way.
James stepped closer, closing the distance between them until he stood just inches away. Clara could smell his cologne, faint and expensive, the kind of scent you pick up in airports and duty-free shops.
“You don’t talk to me like that,” he said quietly, but the threat was unmistakable. “You don’t tell me what’s appropriate. You are a nurse. I am the chief executive of this hospital. If I want this room cleared, it will be cleared. If I want you gone, you will be gone. Do you understand?”
Clara did not step back. Her hands were at her sides, relaxed. Her shoulders were loose. Her voice, when she spoke again, was calm.
“My duty,” she said, “is to protect my patient. I cannot allow anyone, regardless of title, to create a hostile environment at her bedside.”
It took exactly one point eight seconds for everything to change.
For five years, when James reached this level of anger, the sequence was always the same. His hand came up, his palm opened, his body shifted slightly to give the motion force. The person in front of him froze. The impact landed. The gesture did more than sting; it broadcast a message. I can do this to you, and nothing will happen to me.
He repeated the pattern now. His arm moved, a practiced, almost reflexive arc through the air, aimed at Clara’s face.
This time, the pattern broke.
Her left hand rose smoothly, not in a panicked block but in a precise intercept. She caught his wrist mid-swing, at the moment his power was fully committed but not yet delivered. Her fingers curved around bone and tendon with practiced grip, redirecting, not resisting, the momentum.
At the same instant, her right hand moved to the bend of his elbow. Her feet pivoted, her hips turned, and she guided his arm and body past her center line. The movement was fluid, controlled, the kind of motion that comes only after countless repetitions on mats under fluorescent lights in training facilities from North Carolina to California.
His balance went, as surely as if the floor had tilted. His knees buckled. His center of gravity found the path she offered and followed it. In less than two seconds from the moment his hand rose, the CEO of Ridgeview Medical Center was on his knees on the ER floor, his arm captured, his body pinned in a position he could not escape without her consent.
It was not dramatic in the way television fights are dramatic. There was no crash into equipment, no furniture overturned. It was efficient, lean, and unmistakably expert.
The emergency department fell silent.
James tried to wrench his arm free, but the angle made it impossible. Pain flickered in his expression, not sharp enough to constitute injury but clear enough to tell him that continued struggling would lead somewhere he did not want to go. His breathing turned shallow and fast.
“Stop,” he said, the word coming out higher than he intended.
Clara maintained pressure just long enough for him to understand that she was in complete control. Her voice, when she spoke, was level.
“You attempted to strike me,” she said. “I’ve stopped you. You need to calm down.”
Something like panic entered his eyes. Not the kind he’d provoked in others, but genuine fear. For a man who’d spent years striding through rooms unchallenged, the sensation of being physically restrained by someone he considered beneath him was a shock to his system.
“Let me go,” he hissed. “Do you know who I am? You’re finished here. Let me go. Now.”
The last word cracked.
He heard it himself. Everyone in the ER heard it. It sounded less like authority and more like pleading.
“Please,” he added, the word dragged out of him by some instinct deeper than pride, as if his body knew when to trade dignity for freedom before his mind caught up.
Clara held him for three more seconds. Then, in one smooth motion, she released his arm and stepped back, hands open at her sides, posture neutral. Her breathing hadn’t changed. There was no triumphant smile on her face, no visible satisfaction. Only calm.
He scrambled to his feet, his expensive suit rumpled, his hair slightly disordered. His eyes darted around the room, searching for witnesses, for some anchor that would let him reassemble the persona that had ruled this hospital for half a decade.
“I’m calling security,” he said, grasping for familiar ground. “You’re fired. You’ve assaulted me in my own hospital. You’re done here. I’ll see to it that your license never—”
He stopped. No one moved to support him. No one echoed his outrage. The security officers running down the corridor were responding not to his authority but to multiple panic buttons pressed for “physical altercation in ER.”
They arrived within seconds, two of them in navy blue uniforms with RIDGEVIEW SECURITY in white block letters on their shoulders. Behind them came the nursing supervisor and the hospital’s risk management director, both drawn by the same alerts.
“What’s going on here?” the supervisor asked, eyes moving between Clara and James.
“She attacked me,” James said immediately, pointing at Clara. His voice had found more strength, but the tremor was still there if you listened closely. “I came to speak to her, and she assaulted me, completely unprovoked. I want her removed from the building right now.”
Patricia could feel her heart pounding in her throat. For eight years, she had watched people look down at their shoes in these moments, watched complaints dissolve in HR offices. Her mind whispered the familiar advice: stay quiet, stay safe, let it pass.
Then she remembered Clara’s calm voice in the break room, the quiet competence with patients, the hand on Walter’s shoulder, the way she’d stood between Dorothy and the door.
Before she realized she’d made a decision, Patricia stepped forward.
“That’s not what happened,” she said.
Her voice was trembling, but it was loud enough. Everyone heard it.
James turned toward her, disbelief written clearly across his face. No one had contradicted him like that in years. Certainly not in public.
“She was protecting the patient,” Patricia continued, forcing the words out before she could change her mind. “You came in shouting. She explained the situation. You tried to hit her. I saw it. She stopped you. That’s all.”
The ER attending added his voice next, more steady, layered with the authority of a physician licensed in the state of Ohio, a man whose name appeared on insurance forms and quality committees.
“She used minimal force,” he said. “She neutralized an attempted strike. Her actions were appropriate self-defense and in the interests of the patient’s safety.”
The unit coordinator spoke up, her hands still shaking.
“I saw it too. He raised his hand. She stopped him. There was no aggression from her until he tried to hit her.”
A respiratory therapist chimed in. Then a medical student. One by one, people who had been silent for years found their voices. The words came haltingly from some, steadily from others, but they kept coming.
The risk management director listened, her eyes moving from face to face. She had spent years managing incident reports, liability risks, malpractice cases. She had never, in her entire career, seen a room full of staff contradict a hospital CEO in unison.
She turned to Clara.
“Is that accurate?” she asked.
Clara met her gaze. Her eyes were clear.
“Yes,” she said. “I was caring for Mrs. Fletcher, who needed a calm environment. Mr. Comolmes entered in an agitated state. I explained the clinical situation around the CT scanner. He became verbally aggressive. I positioned myself to protect my patient. He raised his hand to strike me. I used a trained defensive technique to stop the strike using the least force necessary. When he was no longer an immediate threat, I released him.”
No drama. No flourish. Just facts.
The security officers looked at each other. Then one of them, the senior, turned to James.
“Sir, we need to ask you to step out of the ER while we take statements,” he said.
“This is my hospital,” James protested. “You don’t order me around—”
The risk management director interrupted softly but firmly.
“For the integrity of the investigation,” she said, “we need everyone’s account taken without pressure. I recommend that you comply.”
There was something in her tone that told him she had already started calculating what this incident meant in terms of liability, regulatory oversight, and headlines in local newspapers.
James looked around the ER again, searching for the familiar reflection of his authority on other people’s faces. He saw none. He saw only witnesses.
He stepped out into the hallway, flanked by security. The automatic doors to the ER slid shut behind him with a soft hiss.
Inside, people exhaled.
Later that night, while statements were still being taken, a detail in Clara’s personnel file reached the risk management office. It had been there from the start, quietly noted, politely ignored by people who assumed prior military service meant nothing more than discipline and reliability.
Eight years active duty in the United States Marine Corps. Combat medic. Multiple deployments. Advanced hand-to-hand combat instructor.
Her record, when they pulled it in full from the federal database, read like something recruiters dreamed of: commendations for courage, letters of appreciation from commanding officers, instructor evaluations praising her control, her judgment under pressure, her ability to train others to defend themselves without escalating situations unnecessarily.
The hospital that had hired her as just another nurse had unknowingly brought in someone who had spent most of her adult life walking into danger on purpose and learning how to bring people back out.
The question everyone at Ridgeview quietly asked in the days that followed was why someone like that had chosen this hospital, of all places.
The answer, when it emerged, reached back three years and hundreds of miles.
Clara’s mother had been treated for cancer at a mid-sized hospital in another state. During one long admission, her roommate had been a woman in her early fifties with a quiet voice and the flat look of someone who had run out of defenses. She had been a nurse once, the woman explained, at a hospital in Ohio. Ridgeview Medical Center.
She told stories in bits and pieces, always lowering her voice when anyone in scrubs walked by. Stories about a CEO who yelled and threatened and sometimes did worse. Stories about complaints that went nowhere, about HR meetings that ended with carefully worded warnings, about colleagues who left nursing altogether because they couldn’t bear the constant tension.
Clara had sat in the uncomfortable visitors’ chair beside her mother’s bed, listening. She filed away the name: Ridgeview Medical Center, near Columbus. The woman eventually discharged, taking her grief and her silence with her.
Clara’s mother died six months later, in a quiet hospice room with an American flag folded on the dresser from her daughter’s service. On one of her last lucid days, she had taken Clara’s hand.
“You’re strong,” she said. “Stronger than you realize. Don’t just use it for yourself. Use it for people who can’t. Promise me.”
Clara gave her the promise. It sat inside her like a compass needle, turning slowly, looking for north.
When she saw a job posting for Ridgeview two years later, she recognized the name immediately. She researched everything she could from a distance: turnover rates, staff reviews, whispers on nursing forums about “a difficult CEO” and “a rough culture.” She looked up board names, local news, anything that could confirm the stories she’d heard.
Then she applied.
She reviewed her defensive training. She refreshed the muscle memory that had once been automatic. She studied employment law, hospital governance, the way U.S. systems were supposed to respond to harassment and violence. She knew she could be fired. She knew she could be blacklisted, quietly, from other hospitals. She knew stepping into Ridgeview was stepping into someone else’s battle.
She went anyway.
In the weeks after the ER incident, the hospital administration tried to treat it as a contained problem, a single event that could be examined, explained, and tidied away. They did not yet understand what Clara had truly broken.
For years, fear had been the air people breathed at Ridgeview. It got into their lungs, their bones, their reflexes. It told them not to speak, not to contradict, not to write things down that might someday be discovered in a subpoena. Fear was how James stayed in power in a country with formal protections and elaborate HR manuals.
In that ER room, for one brief moment, fear had lost.
People had seen a man they’d thought untouchable brought to his knees in less than two seconds. They had heard his voice crack. They had watched him escorted out of a clinical area by security. Those images did something to the stories they’d been telling themselves for years about what was possible and what was not.
When HR scheduled interviews as part of the “internal investigation,” they expected the usual: careful, noncommittal answers. Staff saying they “couldn’t quite see” what had happened, that it had been “confusing,” that “emotions were high.” Instead, they got something else.
Patricia walked into the conference room assigned for interviews on the administrative floor and sat down across from the external investigator brought in by the hospital’s legal team. The investigator was a middle-aged woman with a neutral suit and a notebook already open.
Patricia’s hands shook for the first few minutes. Then she began to talk.
She talked about eight years at Ridgeview. About the day Jennifer disappeared after that meeting near Conference Room B. About the nurse in PACU. About the time James grabbed her own arm so tightly she had to wear long sleeves for a week to hide the faint bruises. She talked about the sick feeling of walking into work every shift, never knowing who would be targeted next.
“Why didn’t you report these incidents at the time?” the investigator asked, not accusing, just gathering facts.
Patricia laughed once, a short, humorless sound.
“To who?” she said. “To HR? They report to him in the end. To the board? We don’t even know their faces. This is America, but in that hospital, it didn’t feel like it. It felt like the law stopped at the lobby and his rules started on the elevators.”
Other staff came in. An ICU nurse described being yelled at so loudly an entire bay heard every word. A tech talked about being written up for “attitude” after raising a concern about patient safety. A doctor, even a doctor, recounted how James had publicly called him incompetent when he questioned an unsafe policy, and how that label had followed him in subtle ways—fewer committee invitations, fewer leadership opportunities.
Former employees started receiving calls. Some refused to talk. Some answered and could not stop once they started. A few had kept journals, little notebooks stuffed in drawers at home, filled with dates and times and short, sharp sentences: May 12: yelled at me in front of family. June 3: slapped L. in hallway. July 19: called K. “replaceable” when she asked for safe staffing. They had written everything down not just for lawsuits they never filed, but to prove to themselves that what they had endured was real.
One name surfaced that caught the investigator’s attention: a nurse from a different hospital in another state where James had worked before Ridgeview. That nurse, Michelle Rodriguez, told a story that sounded painfully familiar. Same temper. Same pattern. Same settlements.
Individual incidents, when taken alone, could be explained away. Together, they painted a picture so clear even people determined not to see it would have struggled to look past it.
The hospital’s legal team read the preliminary report and understood immediately that this was no longer just an internal management issue. It was a legal exposure measured not just in dollars, but in regulatory scrutiny, media coverage, and the potential interest of the state attorney general’s office.
The board, which had spent years congratulating itself on Ridgeview’s financial performance and expansion in the regional U.S. market, could no longer ignore the storm at their doorstep.
They called an emergency meeting.
The boardroom on the top floor had a sweeping view of the city, the kind of skyline that looked good in annual reports: church steeples, a stadium, a river reflecting lights. The long table was set with water pitchers and notepads. The atmosphere felt heavier than any meeting they had held in recent memory.
The external investigator presented her findings in measured tones. She went through timelines, corroborated incidents, patterns of behavior, legal definitions of harassment and assault. She did not use dramatic language. She didn’t need to. The facts were dramatic enough.
When she finished, one of the board members asked a question that landed like something from another world.
“How much of this is just a difference in management style?” he asked. “Healthcare is tough in this country. You have to be firm to keep a hospital afloat.”
The investigator looked at him steadily.
“In the United States,” she said, “management style does not include physical aggression. It does not include slapping employees, grabbing them hard enough to leave marks, or creating a documented pattern of intimidation and retaliation. That’s not a style. That’s misconduct.”
They invited Clara to speak.
She entered the room in her navy scrubs, badge clipped to her chest, hair still pulled back. She could have worn something else, but she’d come straight from the unit, and the truth was, this was who she was at Ridgeview: a bedside nurse.
She sat at the far end of the table while twelve people in suits watched her. Some of them had likely voted for James’ compensation packages. Some had applauded his speeches about fiscal responsibility and strategic partnerships. Some had never stepped foot on a med–surg unit except for photo opportunities.
“Walk us through what happened in the emergency department,” the board chair said.
Clara did. She described Dorothy’s admission, the trauma case in CT, the clinical reasoning behind the delay. She described James’ entrance, his questions, his tone. She described his hand rising, and the technique she used to stop him.
“Did you intend to harm him?” one board member asked.
“No,” she said. “My intent was to prevent harm. To myself, and to my patient. The technique I used is designed to control, not injure. I released him as soon as he stopped moving aggressively.”
“Would you do it again?” another member asked.
“If the exact same situation occurred again,” she said, “and a person in authority attempted to strike me while I was standing between them and a vulnerable patient, yes. My duty of care wouldn’t change because of a title.”
They asked about her past service. She answered simply. Yes, she had been a Marine. Yes, she had deployed. Yes, she had taught defensive tactics. No, she had never used her training to initiate violence in a civilian setting. She had used it to protect herself and others when necessary.
When they dismissed her, she left the room as calmly as she had entered.
The board went into closed session. They talked about contracts, severance clauses, leadership transitions. They spoke in the careful language of people who understood lawyers were listening, even if no attorney sat at the table.
In the end, the decision took less time than any of them expected.
They reconvened, called James in, and told him he was terminated for cause.
There were formal words about policy violations, about conduct unbecoming a leader in a U.S. healthcare institution, about breaches of trust. There were references to documentation, investigations, corroborated accounts. There was language about “no severance, effective immediately.”
James stared at them as if they were speaking a foreign language. For years, he had been the one reading termination scripts to others. Now, the words fell on him like cold water.
“You’re going to ruin this hospital,” he said, trying one last time to pivot. “You’re going to send a message that staff can undermine leadership whenever they don’t like decisions. You’re rewarding insubordination.”
“We’re sending a message,” the board chair replied, “that no one in this building is above basic standards of behavior or the law. Not even the CEO.”
Security escorted James from his office that afternoon. They walked beside him as he carried a single cardboard box filled with framed degrees, a few family photos, a coffee mug from a conference in Chicago. The walk through the administrative corridor felt longer than it ever had.
Some staff watched from open office doors. No one said anything. No one reached out to shake his hand. The elevator ride to the ground floor was quiet. When the doors opened to the lobby, he stepped out, pausing once to glance back at the seal of Ridgeview Medical Center etched into the tile.
Outside, the American flag still fluttered over the entrance. The sky was a clear, bright blue that would look good in a tourism brochure. He walked to his car, put the box in the trunk, and left the parking lot for the last time as Ridgeview’s chief executive.
Inside, the air in the hospital shifted.
People did not break into applause. This wasn’t a movie. Patients still needed medications, monitors still beeped, labs still came back, families still worried in waiting rooms. But there was a lightness, a subtle change in the way people held their shoulders or met each other’s eyes.
In the break room on 4 North, Patricia sat down next to Clara with a cup of coffee she’d barely had time to pour.
“He’s really gone,” Patricia said. “They terminated him. For cause.”
Clara watched the steam curl up from her own cup.
“I heard,” she said.
“This place feels different,” Patricia added. “Not fixed. But different.”
“Fear doesn’t leave overnight,” Clara said. “It takes time to unlearn it. But it can be done.”
The processes that followed were slow and bureaucratic, the way such things always are in American systems.
Several nurses, encouraged by the board’s decision and the external investigation, filed formal complaints with the local prosecutor’s office about past incidents involving physical aggression. Attorneys reviewed documentation, medical records, past HR notes. A criminal case opened, then widened. There were discussions of charges, negotiations, motions in courtrooms where wood-paneled walls had seen a thousand lives derailed.
In parallel, state regulators took notice. Licensing boards, both for medicine and for hospital administration, began to examine James’ record more closely. The narrative that had once painted him as a decisive leader who turned struggling hospitals around now had an inconvenient second column: staff turnover, complaints, settlement agreements.
Civil suits appeared as well. Some were resolved quietly. Some lingered. None would rewrite the past for the people who had left nursing entirely or who still woke up at night thinking about the day they’d stood frozen while someone in authority did something unforgivable.
Ridgeview, for its part, had to decide what kind of hospital it wanted to be now that the man who had shaped its culture through fear was gone.
They appointed an interim CEO, a physician–administrator who had spent much of her career talking about workplace dignity, not just profit margins. She walked the units not to intimidate but to listen, standing at nurse stations with a notepad, asking, “What do you need that you’re not getting?” and “How can we make it safer for you to speak up when something’s wrong?”
Clara did not suddenly become the center of the hospital. She still had patients, still did night shifts, still charted, still argued with pharmacy about stat meds and coaxed anxious family members into resting for a few hours. But people looked at her differently now.
They began inviting her to committees: a workplace safety group, an advisory council on staff well-being, an ethics meeting where someone suggested establishing a formal pathway for reporting harassment and violence that didn’t run solely through HR. She accepted the invitations carefully, wary of becoming a symbol instead of a worker.
When she spoke in those meetings, she did so plainly.
“You can write policies all day,” she said once, sitting in a conference room that still smelled faintly of dry-erase markers and coffee. “If people don’t believe they’ll be enforced fairly, they won’t use them. You have to prove, over and over, that when someone reports something, it will be taken seriously and they won’t be punished for it.”
They built new reporting mechanisms, some anonymous, some confidential but traceable. They offered training on de-escalation and respectful communication—not just for frontline staff, but for physicians and managers. They added clear language to codes of conduct about zero tolerance for physical aggression, no matter who initiated it.
The changes were not magic. Some people were skeptical, and with reason. They had seen promises come and go. But time and consistency did what speeches could not. When staff saw a manager disciplined for yelling at a tech, when they saw a physician required to attend training after a pattern of rude behavior, when they watched a complaint from a housekeeper investigated with the same seriousness as one from a doctor, something began to heal.
Turnover slowed. Exit interviews included fewer mentions of “hostile environment” and “toxic culture.” New hires began to come not just because Ridgeview paid competitive wages in an American market that desperately needed nurses, but because word had spread that someone had finally drawn a line there and the hospital had honored it.
Clara’s own path shifted gradually. Six months after the incident, she was offered a nurse manager role. It meant more meetings, fewer patients, more responsibility. She hesitated, missing the pure focus of bedside work. In the end, she accepted, in part because she knew that good managers could shield their staff in ways she’d once wished for herself.
She approached leadership the way she’d approached everything else: with quiet steadiness. She listened more than she talked. She backed her nurses when they raised clinical concerns. She pushed back against staffing ratios that put them or patients at risk. When someone complained about a doctor’s tone, she didn’t dismiss it as sensitivity; she addressed it.
Years later, the hospital that had once been known in whispered online forums as “a rough place to work in Ohio” started showing up in different kinds of conversations. Articles in healthcare journals mentioned Ridgeview as an example of cultural transformation after leadership abuse. Conferences invited their people to talk about practical changes, not just slogans.
Clara eventually became Chief Nursing Officer, overseeing nursing practice across the entire system. She kept her old badge in a drawer in her office, the one from her first week on 4 North, as a reminder of where she started and why she had come.
On some days, walking through the halls, she would pass the ER doorway where everything changed. The floor looked the same. The paint on the walls had been touched up, but not dramatically. The CT scanner still hummed in its room. The U.S. flag still waved outside.
She thought sometimes of Dorothy, who recovered enough function to complain gently about how noisy the hospital was and to ask whether her husband had made sure donations went to the nursing education fund. She thought of Walter, who told every nurse who walked into his room that they should listen to “the Marine,” because she understood things.
She thought of Jennifer and Michelle and Karen and all the names she knew and the ones she didn’t, the nurses and techs and assistants who had endured what should never be part of anyone’s job.
She thought of her mother, who had asked her to use her strength for more than herself.
People sometimes asked Clara, in formal interviews or casual conversations, if she had been afraid that day in the ER.
“Of getting hurt?” she would say. “No. I knew what I could do if I had to. Of what would happen afterward? Yes. There are always consequences when you stand up to power.”
“And was it worth it?” they would ask.
She would think of Ridgeview now: of nurses who argued with doctors when orders didn’t make sense, of CNAs who reported unsafe conditions without fear, of residents who apologized when they snapped at staff during stressful nights, of a culture where people believed, deep down, that their dignity mattered.
“Every second,” she would answer.
The story people told about Ridgeview changed over time. It stopped being just the story of a man who had used fear to build his own fragile throne and started being the story of the day that throne cracked in less than two seconds on an ER floor in an American hospital.
It became the story of how one quiet nurse, who had walked through war zones before she ever put on a navy scrub top, kept a promise made in a hospice room and showed a building full of frightened people that fear is not the same as fate.
And in corridors that had once echoed with slammed doors and raised voices, it became, slowly and imperfectly but undeniably, the story of how courage spread.
News
On the way to the settlement meeting, i helped an old man in a wheelchair. when he learned that i was also going to the law firm, he asked to go with me. when we arrived, my sister mocked him. but her face turned pale with fear. it turned out the old man was…
The invoice hit the marble like a slap. “You have twenty-four hours to pay forty-eight thousand dollars,” my sister said,…
After my parents’ funeral, my sister took the house and handed me a $500 card my parents had left behind, like some kind of “charity,” then kicked me out because I was adopted. I felt humiliated, so I threw it away and didn’t touch it for five years. When I went to the bank to cancel it, the employee said one sentence that left me shocked…
A plain white bank card shouldn’t be able to stop your heart. But the moment the teller’s face drained of…
My sister locked me inside a closet on the day of my most important interview. I banged on the door, begging, “This isn’t funny—open it.” She laughed from outside. “Who cares about an interview? Relax. I’ll let you out in an hour.” Then my mom chimed in, “If not this one, then another. You’d fail anyway—why waste time?” I went silent, because I knew there would be no interview. That “joke” cost them far more than they ever imagined.
The first thing I remember is the smell. Not the clean scent of morning coffee or fresh laundry drifting through…
On Christmas Eve, my seven-year-old found a note from my parents: “We’re off to Hawaii. Please move out by the time we’re back.” Her hands were shaking. I didn’t shout. I took my phone and made a small change. They saw what I did—and went pale…
Christmas Eve has a sound when it’s about to ruin your life. It isn’t loud. It isn’t dramatic. It’s the…
On my 35th birthday, I saw on Facebook that my family had surprised my sister with a trip to Rome. My dad commented, “She’s the only one who makes us proud.” My mom added a heart. I smiled and opened my bank app… and clicked “Withdraw.
The candle I lit on that sad little grocery-store cupcake didn’t glow like celebration—it glowed like evidence. One thin flame,…
My son-in-law and his father threw my pregnant daughter off their yacht at midnight. She hit something in the water and was drowning in the Atlantic. I screamed for help, but they laughed and left. When the Coast Guard pulled her out three hours later, I called my brother and said, “It’s time to make sure they’re held accountable.”
The Atlantic was black that night—black like poured ink, like a door slammed shut on the world. Not the movie…
End of content
No more pages to load